When Crystal Bowersox was competing on Season 9 of American Idol in 2010, she kept her type 1 diabetes a secret. She didn’t want producers or competitors treating her any differently or giving her special treatment. That changed when she into DKA (diabetic ketoacidosis) and had to be hospitalized, almost leaving the show.

A decade later she tells everyone about her diabetes because, the truth is, diabetics do need special treatment.
She told the Extreme Hypoglycemia Summit hosted by Lilly Canada in January a story about going low on stage in front of an audience. She had to trust that her guitar player would recognize the signs, or her manager would be backstage watching her numbers, and be ready to help. As a single mom, she has had to train her son to be her caregiver. He’s nearly 11 and can recognize the signs of a low and is empowered to be someone’s hero.
She has a team of people ready to help when and if she can’t help herself, something all diabetics need.
NO SUCH THING AS PERFECT
When you have type 1 diabetes, your pancreas doesn’t produce insulin to turn carbohydrates into energy in your body. So you have to act as a pancreas, injecting yourself with insulin while accounting for exercise, food intake, and other mitigating factors. It’s a complicated equation that must be performed multiple times throughout the day.
Diabetics are trained to keep their blood sugar numbers to the low side of average because going higher can mean long term damage from retinopathy and neuropathy. But the lower the average, the greater the risk of having a bad low that can result in unconsciousness.
It’s a precarious dance.

Dr. Ian Blumer also spoke at the Extreme Hypoglycemia Summit in January. He explained there is “no such thing as perfect when treating diabetes.” Patients can do finger pricks to check their blood sugar, but that’s just a moment in time. With most people checking about 3x a day, that’s getting data for 3 minutes out of an entire day.
Continuous glucose monitors (CGM) are game-changers for diabetics but only 20% of T1D use them. So there will be inevitable swings in blood sugar numbers that aren’t always predictable and can sometimes lead to a severe low called hypoglycemia.
It’s this unexpected, and serious, low that worries Robert Oringer, a father of two type 1 sons.
“When you’re diagnosed with type 1 diabetes, or when that physician says to anyone with diabetes ‘I’m putting you on insulin,’ you have that first diagnosis. What nobody speaks about is what I call the second diagnosis: hypoglycemia,” he explained.
“You’ve been diagnosed with this second thing that’s going to hang over you all of the time. I refer to it sometimes as the plague of hypoglycemia, because every day, all the time, you’re thinking about hypoglycemia and how to avoid it.”
And when you have type 1 kids, thinking about hypoglycemia can become all-consuming. You can’t rely on a 3 or 5 or 9-year-old to accurately track their blood sugar throughout the day – can you? And what if they go low, will the people who don’t live with a diabetic be able to recognize the signs and act properly in an emergency?
IT TAKES A VILLAGE
I was reading through an online diabetes community recently and my heart sank as a parent told of a meeting with her son’s school administration about his diabetes. He’s 6 years old, in Grade 1 and, like all diabetics, relies on someone to help should he go low.
Except the school wasn’t willing to help.
“I was informed that they do not administer glucagon and they will not check my 6-year-old’s blood sugar levels,” the mother shared. “They will give him dex tabs for a low… but how are they suppose to check his blood sugar 15 minutes later to see if they were enough?”
“I am just worried about my 6-year-old. I work 45 minutes away, my husband works in a factory so can’t always have his cell on him… how will the school handle the low? We have no family that can help us out.”
And right there you have the part of diabetes that nobody ever talks about outside the diabetes community – the worry.
WHO HAS YOUR BACK?
A ‘run of the mill low’ can often be treated by taking something with a quick-acting sugar.
“The only thing kids knew about me in school was that Zoeie gets to eat sugar,” the panel’s moderator, Zoeie Major-Orfao, told the summit. One of the kids in her class, envious of the candy Zoeie took when she was experiencing a low, put a red stain on a tissue and proclaimed “I have diabetes too,” in hopes of getting in on the candy train.
This is why diabetics usually carry a bag of candy, or a juice box, or glucose tabs. But if the low is severe, they’re helpless.
Severe hypoglycemia is an emergency where the person with diabetes is no longer able to treat themselves. They could be unresponsive, have a seizure, be unconscious, or unable to do something as simple as sip juice through a straw or chew some tabs.
Severe hypoglycemia is life-threatening and needs immediate treatment, traditionally through glucagon, which requires a needle and vial contraption that many diabetics carry with them at all times.
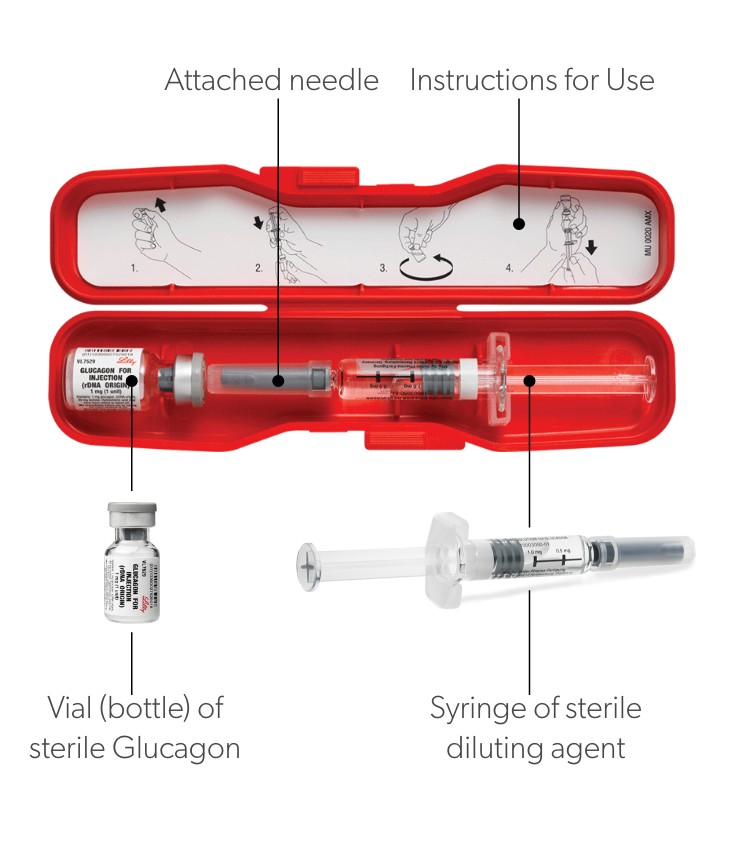
It’s not a simple process to properly dilute the glucagon and administer the shot to someone you may or may not know, who may or may not be conscious, or having a seizure. It’s straight-up intimidating.
And yet a diabetic with severe hypoglycemia will rely on someone to perform this perfectly to have their back.
And that’s why Robert Oringer, the father of two sons with type 1 diabetes, a well-known face in the diabetes community as the creator of Dex4 glucose tabs, sought to find a way to take the fear away and to make treating severe hypoglycemia simpler.
BAQSIMI IS A GAME CHANGER
As Oringer worked on a replacement for the glucagon needle, he realized that he needed to think less about the patient, and more about the person helping them.
“It’s not the drug that has your back,” he explained. “It’s the people that have to deliver it that have your back.”
He wanted his solution to be non-invasive, so no needle. It needed to be easy to use, easy to teach, and easy to carry. And that’s when his team settled on a nasal administration he originally dubbed Schnozagon before brainstorming a better name, Baqsimi, to embrace his idea that this was to help those helping a diabetic in an emergency.
“The way I share it, someone that is put on insulin, they know, in their heads, who will have their back,” says Oringer. “Now, with a puff in the nose, I think we enable a level of confidence, not just for the person who uses insulin to feel that others have their back, but for the people that love or care for them to feel they can have someone’s back.”
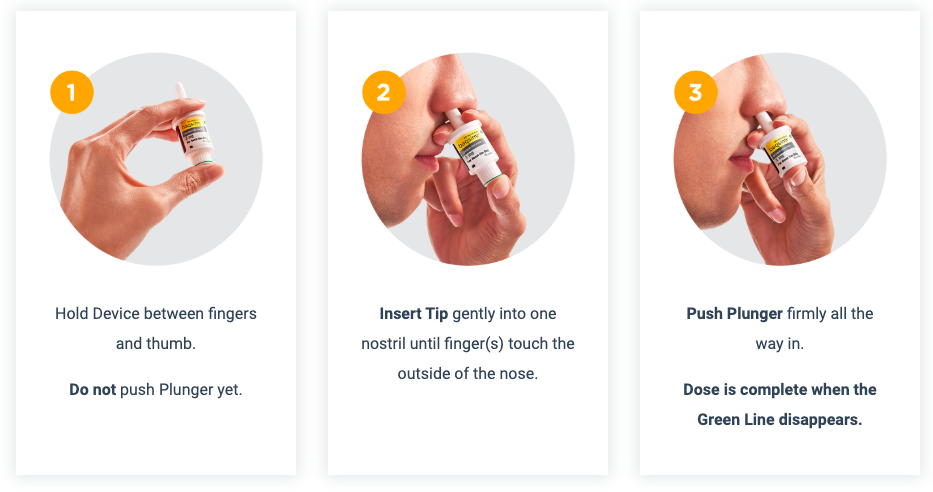
Baqsimi is powdered glucagon stored in a small plastic container about the size of your thumb. You put it in the patient’s nose and then press the bottom firmly to release a fine mist of glucagon to the patient.
That’s it. No needle, no mixing. It’s a simple as taking any nasal spray.
AWARENESS MATTERS
The label for Baqsimi reads “for treatment of severe blood sugar,” but when Oringer originally envisioned the Baqsimi package label, he thought it could say, in big letters, Insulin Insurance.
“In my head, the version I also imagined and that I’m maybe most proud of would say, Hypoglycemia Discussion Enabler, because the simplicity of nasal delivery makes it so easy to discuss hyperglycemia rescue.
All the people that you didn’t talk to because you would’ve – and I’ll use a strong word – traumatized them by displaying the kit, they are now enabled. They can puff it in your nose. That gives people confidence and reduces fear.”

Awareness matters for diabetics, they need support and understanding from the community at large to step in and save their life, if needed. Baqsimi makes it easier for everyone to be a hero, and to have a diabetics’ back – it’s almost as easy as colouring a tissue to try to get some candy from the teacher.

Thanks to Eli Lilly Canada for inviting me to the Severe Hypoglycemia Summit to learn more about Baqsimi and to meet some inspiring young Canadians living with type 1 diabetes.
I’m proud to have your back any time you need.
This post is sponsored by Eli Lilly Canada

For more information about Baqsimi and how you can be prepared for an unexpected severe hypoglycemic event, please visit, www.baqsimi.ca.
About Baqsimi
Baqsimi is a portable, ready-to-use form of glucagon which requires no reconstitution or priming. It is administered in a single fixed dose of 3 mg which is sprayed in the nose, where it is absorbed. Baqsimi does not need to be refrigerated and can be stored at temperatures up to 30°C/86°F in its shrink-wrapped tube.
Baqsimi is indicated for the treatment of severe hypoglycemic reactions in people 4 years old and above when impaired consciousness precludes oral carbohydrates, which may occur in the management of insulin-treated patients with diabetes mellitus. The formulation was discovered in Canada.
 About Lilly Canada
About Lilly Canada
Eli Lilly and Company is a global healthcare leader that unites caring with discovery to make life better for people around the world. We were founded more than a century ago by Colonel Eli Lilly, who was committed to creating high-quality medicines that meet people’s needs, and today we remain true to that mission in all our work. Lilly employees work to discover and bring life-changing medicines to people who need them, improve the understanding and management of disease, and contribute to our communities through philanthropy and volunteerism.
Eli Lilly Canada was established in 1938, the result of a research collaboration with scientists at the University of Toronto which eventually produced the world’s first commercially-available insulin. To learn more about Lilly Canada, please visit www.lilly.ca

Dad. Broadcaster. Writer.
Three time Guinness World Record Holder.
I run the world for Team Diabetes.
